Concept mapping, a visual tool that organizes and represents knowledge, has become increasingly popular in nursing education and practice. Far beyond simple note-taking, concept maps facilitate deep learning, critical thinking, and a holistic understanding of complex patient scenarios. This article will explore the power of concept mapping in nursing, delving into various examples that demonstrate its application across different clinical situations, educational levels, and professional development goals.
What is a Concept Map and Why Use It in Nursing?
At its core, a concept map is a diagram that illustrates relationships between concepts. These concepts, often represented by boxes or circles, are linked by lines or arrows, with connecting words or phrases that explain the nature of the relationship. The structure is hierarchical, with broader, more general concepts at the top, branching down to more specific and detailed concepts.
The benefits of using concept mapping in nursing are numerous:
- Enhanced Learning: Concept maps encourage active learning by forcing students to actively organize and synthesize information. This active engagement leads to better retention and recall of knowledge.
- Improved Critical Thinking: By visualizing the connections between concepts, nurses can analyze complex situations, identify patterns, and make more informed decisions.
- Holistic Understanding: Concept maps promote a holistic perspective, allowing nurses to see the "big picture" and understand how different factors influence a patient’s health.
- Effective Communication: Concept maps provide a clear and concise visual representation of complex information, facilitating communication between healthcare professionals and patients.
- Better Problem-Solving: Concept maps can be used to analyze problems, identify potential solutions, and evaluate the effectiveness of interventions.
- Personalized Learning: Concept mapping allows individuals to learn at their own pace and in a way that best suits their learning style.
- Improved Clinical Judgement: Through the process of connecting concepts and identifying relationships, nurses develop stronger clinical judgement skills, leading to safer and more effective patient care.
Concept Map Nursing Examples: A Deep Dive
Let’s explore some concrete examples of how concept maps can be applied in various nursing contexts:
1. Nursing Process and Patient Assessment:
A fundamental application of concept mapping in nursing is to structure the nursing process and patient assessment. Imagine a patient presenting with chest pain. A concept map could begin with the central concept of "Chest Pain" and branch out into the following areas:
- Assessment: This branch would further subdivide into:
- Subjective Data: Patient’s description of pain (location, intensity, duration, characteristics), associated symptoms (nausea, shortness of breath, dizziness), medical history, medications, allergies.
- Objective Data: Vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation), physical examination findings (auscultation of heart and lungs, palpation of chest), ECG results.
- Nursing Diagnoses: Based on the assessment data, potential nursing diagnoses could be identified, such as:
- Acute Pain: Related to myocardial ischemia as evidenced by patient report of chest pain and ECG changes.
- Decreased Cardiac Output: Related to decreased myocardial contractility as evidenced by hypotension and shortness of breath.
- Anxiety: Related to fear of death as evidenced by patient verbalization of fear and restlessness.
- Planning: This branch would outline specific, measurable, achievable, relevant, and time-bound (SMART) goals for each nursing diagnosis. For example:
- Acute Pain: Patient will report pain level less than 3 on a scale of 0-10 within 1 hour of medication administration.
- Decreased Cardiac Output: Patient will maintain a blood pressure within normal limits within 2 hours of initiating treatment.
- Anxiety: Patient will verbalize decreased anxiety and demonstrate relaxation techniques within 30 minutes of intervention.
- Implementation: This branch would detail the nursing interventions required to achieve the planned goals. For example:
- Acute Pain: Administer prescribed pain medication, monitor pain level, provide comfort measures (positioning, relaxation techniques).
- Decreased Cardiac Output: Administer oxygen, monitor vital signs, administer prescribed medications (e.g., diuretics, vasodilators), elevate legs.
- Anxiety: Provide emotional support, explain procedures, teach relaxation techniques (deep breathing, guided imagery), provide a calm environment.
- Evaluation: This branch would assess the effectiveness of the interventions and determine if the goals have been met. It would also identify areas for improvement and modifications to the care plan.
This example demonstrates how a concept map can structure the entire nursing process, providing a comprehensive framework for patient care.
2. Pathophysiology and Disease Management:
Concept maps are particularly useful for understanding complex pathophysiology and disease processes. Consider a patient with diabetes mellitus. A concept map could start with "Diabetes Mellitus" as the central concept and branch out into the following areas:
- Pathophysiology: This branch would explain the underlying mechanisms of the disease, including:
- Type 1 Diabetes: Autoimmune destruction of pancreatic beta cells leading to insulin deficiency.
- Type 2 Diabetes: Insulin resistance and impaired insulin secretion.
- Hyperglycemia: Elevated blood glucose levels due to insulin deficiency or resistance.
- Glycosuria: Excess glucose in the urine.
- Polyuria: Increased urination due to osmotic diuresis.
- Polydipsia: Increased thirst due to dehydration.
- Polyphagia: Increased hunger due to cellular starvation.
- Complications: This branch would outline the potential complications of diabetes, including:
- Microvascular Complications: Retinopathy, nephropathy, neuropathy.
- Macrovascular Complications: Coronary artery disease, peripheral artery disease, stroke.
- Diabetic Ketoacidosis (DKA): A life-threatening complication characterized by hyperglycemia, ketosis, and acidosis.
- Hyperosmolar Hyperglycemic State (HHS): Another life-threatening complication characterized by severe hyperglycemia and dehydration.
- Management: This branch would detail the various aspects of diabetes management, including:
- Lifestyle Modifications: Diet, exercise, weight management.
- Medications: Insulin, oral hypoglycemic agents.
- Blood Glucose Monitoring: Regular self-monitoring of blood glucose levels.
- Education: Patient education on diet, exercise, medication management, and complication prevention.
By visually connecting these concepts, nurses can develop a deeper understanding of diabetes and its management, leading to more effective patient education and care.
3. Pharmacology and Medication Administration:
Concept maps can also be used to understand the mechanisms of action, indications, contraindications, and side effects of medications. For example, a concept map for "Morphine" could include the following:
- Mechanism of Action: Binds to opioid receptors in the central nervous system, reducing the perception of pain.
- Indications: Moderate to severe pain relief.
- Contraindications: Respiratory depression, hypersensitivity, acute asthma.
- Side Effects: Respiratory depression, constipation, nausea, vomiting, sedation, hypotension.
- Nursing Considerations: Monitor respiratory rate and depth, assess pain level, administer stool softeners, educate patient about potential side effects.
This approach allows nurses to organize and synthesize information about medications, ensuring safe and effective administration.
4. Clinical Simulations and Case Studies:
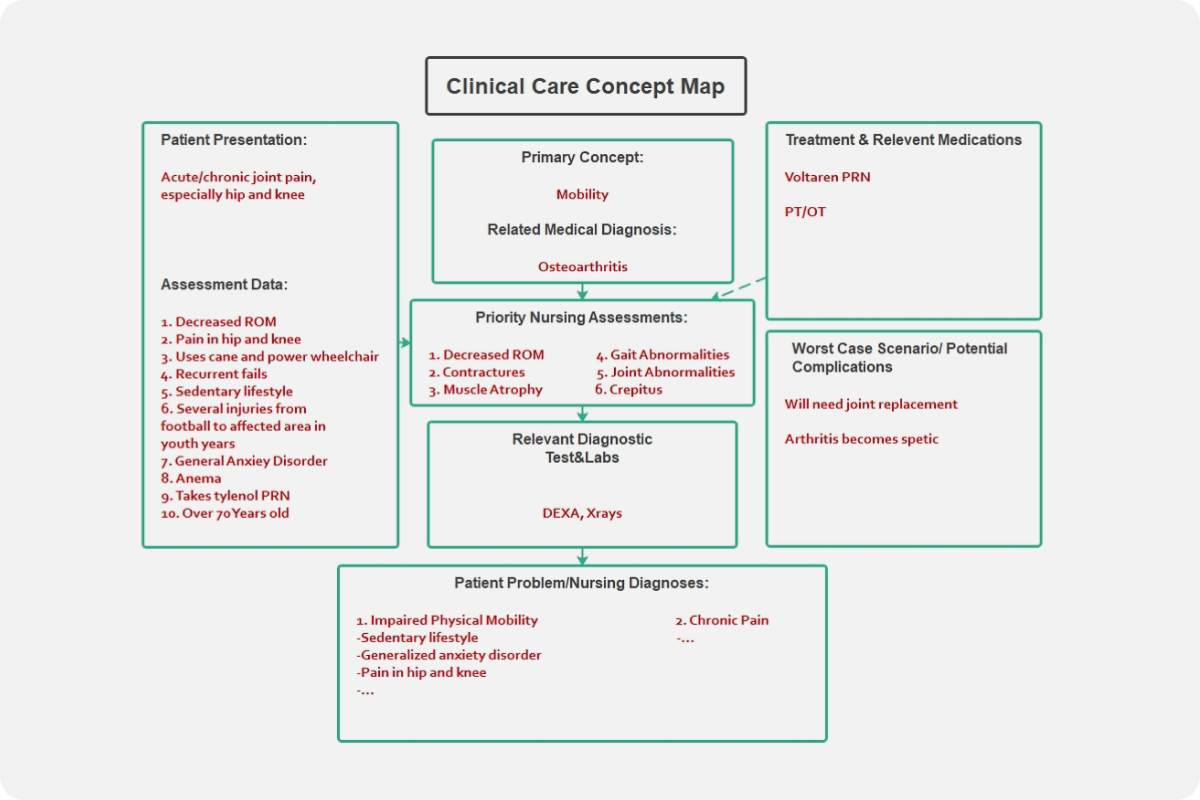
Concept maps are invaluable tools for analyzing clinical simulations and case studies. After reviewing a patient scenario, students can create a concept map to:
- Identify Key Problems: Prioritize the most critical issues facing the patient.
- Develop Nursing Diagnoses: Formulate appropriate nursing diagnoses based on the patient’s assessment data.
- Plan Interventions: Outline specific nursing interventions to address the identified problems.
- Evaluate Outcomes: Assess the effectiveness of the interventions and identify areas for improvement.
This process helps students develop critical thinking skills and apply their knowledge to real-world clinical situations.
5. Patient Education:
Concept maps can be simplified and tailored for patient education. Visual aids are particularly helpful for patients with limited literacy or those who learn best visually. A simple concept map explaining "Heart Failure" could include the following:
- Heart Failure: The heart cannot pump enough blood to meet the body’s needs.
- Symptoms: Shortness of breath, fatigue, swelling in the legs and ankles.
- Causes: High blood pressure, heart attack, heart valve problems.
- Treatment: Medications, diet, exercise, lifestyle changes.
By presenting information in a clear and concise visual format, nurses can empower patients to better understand their condition and actively participate in their care.
Creating Effective Concept Maps:
While the benefits of concept mapping are clear, creating effective maps requires practice and attention to detail. Here are some tips for creating impactful concept maps:
- Start with a Central Concept: Identify the main topic or issue you want to explore.
- Identify Key Concepts: Brainstorm a list of relevant concepts related to the central concept.
- Organize Concepts Hierarchically: Place broader, more general concepts at the top and more specific concepts below.
- Use Linking Words and Phrases: Clearly explain the relationships between concepts using verbs, prepositions, or phrases.
- Use Color and Visual Cues: Employ color coding, different shapes, and other visual cues to enhance clarity and organization.
- Revise and Refine: Concept maps are not static documents. Revise and refine them as you learn more and gain a deeper understanding of the topic.
- Utilize Software Tools: Several software programs and online tools are available to facilitate concept map creation.
Conclusion:
Concept mapping is a powerful tool that can enhance learning, improve critical thinking, and promote a holistic understanding of complex patient scenarios in nursing. By visualizing the connections between concepts, nurses can develop stronger clinical judgment skills, provide more effective patient care, and contribute to a safer and more efficient healthcare system. Whether used in the classroom, clinical setting, or for personal learning, concept mapping offers a valuable framework for unlocking understanding and achieving excellence in nursing practice. The examples provided illustrate the diverse applications of this technique, encouraging nurses to embrace concept mapping as a vital tool in their professional journey.